Hypoplastic Left Heart Syndrome
Contents:
However, oxygen-poor blue blood returning to the heart from the lower body through the inferior vena cava will still mix with oxygen-rich red blood in the left heart and travel to the body, so the child will remain cyanotic. This operation helps create some of the connections necessary for the final operation, the Fontan procedure.
This operation allows all the oxygen-poor blue blood returning to the heart to flow into the pulmonary artery and lungs, greatly improving the oxygenation of the blood. The Glenn shunt, connecting the superior vena cava to the right pulmonary artery, is left in place. A second connection is made directing blood from the inferior vena cava to the right pulmonary artery as well. This connection can be created in slightly different variations, depending on the method your child's surgeon prefers, and what is best for your child. After surgery, infants will return to the intensive care unit ICU to be closely watched during recovery.
The open chest prevents compression of the heart by the rib cage.
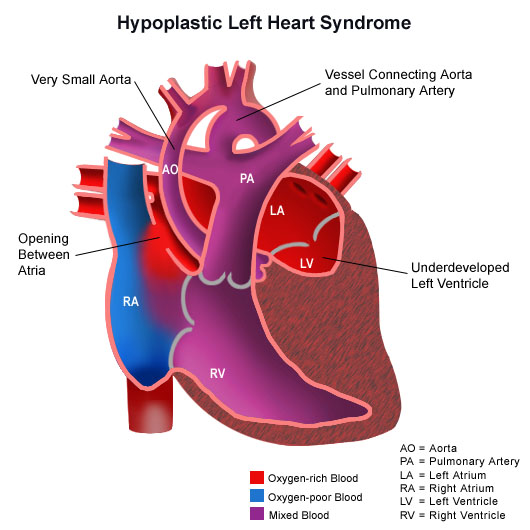
Hypoplastic (pronounced hi-puh-PLAS-tik) left heart syndrome or HLHS is a birth defect that affects normal blood flow through the heart. Overview. Hypoplastic left heart syndrome is a complex and rare heart defect present at birth (congenital). The left side of the heart is critically.
While your child is in the ICU, special equipment will be used to help him or her recover, and may include the following:. A machine that helps your child breathe while he or she is under anesthesia during the operation. A small, plastic tube is guided into the windpipe and attached to the ventilator, which breathes for your child while he or she is too sleepy to breathe effectively.
- Best of Friends.
- Hypoplastic Left Heart Syndrome.
- Hypoplastic left heart syndrome!
- Navigation menu.
- What is hypoplastic left heart syndrome?;
Small, plastic tubes inserted through the skin into blood vessels to provide IV fluids and important medicines that help your child recover from the operation. A specialized IV placed in the wrist or other area of the body where a pulse can be felt, that measures blood pressure continuously during surgery and while your child is in the ICU.
A small, flexible tube that keeps the stomach drained of acid and gas bubbles that may build up during surgery. A small, flexible tube that allows urine to drain out of the bladder and measures how much urine the body makes. This helps determine how well the heart is functioning.
Immediately after surgery, the heart will be a little weaker than it was before, and the body may start to hold onto fluid, causing swelling and puffiness.
Hypoplastic Left Heart Syndrome / Norwood Procedure
Diuretics may be given to help the kidneys to remove excess fluid from the body. A drainage tube may be inserted to keep the chest free of blood that would otherwise accumulate after the incision is closed. Bleeding may occur for several hours, or even a few days after surgery. A machine that constantly displays a picture of your child's heart rhythm, and monitors heart rate, blood pressure, and other values. Your child may need other equipment not mentioned here to provide support while in the ICU, or afterwards.
Page not available
The hospital staff will explain all of the necessary equipment to you. The staff will also be asking for your input as to how best to soothe and comfort your child. After discharge from the ICU, your child will recuperate on another hospital unit before going home. You will learn how to care for your child at home before your child is discharged.
Your child may need to take medications for a while, and these will be explained to you. The staff will give you instructions regarding medications, activity limitations, and follow-up appointments before your child is discharged. Infants who spent a lot of time on a ventilator, or who were fairly ill while in the ICU, may have trouble feeding initially.
These babies may have an oral aversion; they might equate something placed in the mouth, such as a pacifier or bottle, with a less pleasant sensation, such as being on the ventilator. Some infants are just tired, and need to build their strength up before they will be able to learn to bottle-feed. Strategies used to help infants with nutrition include the following:.
High-calorie formula or breast milk.
In this procedure, a stent is placed in the ductus arteriosus to maintain its patency, and bands are placed over both the left and right pulmonary artery branches to limit pressure and over-circulation to the lungs. This operation helps create some of the connections necessary for the final operation, the Fontan procedure. Regular follow-up care at a center offering highly-specialized congenital cardiac care should continue throughout the individual's lifespan. Initially, your child may be placed on oxygen, and possibly even on a ventilator, to assist with breathing. The patent ductus arteriosus, a normal structure in the fetus, is often the only pathway through which blood can reach the body from the heart.
Feedings given through a small, flexible tube that passes through the nose, down the esophagus, and into the stomach, that can either supplement or take the place of bottle-feedings. Infants who can drink part of their bottle, but not all, may be fed the remainder through the feeding tube. Infants who are too tired to bottle-feed at all may receive their formula or breast milk through the feeding tube alone. Pain medications, such as acetaminophen or ibuprofen, may be recommended to keep your child comfortable at home.
If any special treatments are to be given at home, the nursing staff will ensure that you are able to provide them, or a home health agency may assist you. Without intervention, most infants with HLHS will not survive longer than a few days to a few weeks. Heart transplantation is an option, but because of the difficulty in obtaining a donor heart for an infant, the series of surgical procedures described above is most often recommended.
The first-stage procedure poses the highest risk for poor outcomes and death. Some specialized centers where a greater number of procedures are done have achieved survival rates that are higher than at centers where fewer procedures are done. Survival rates are higher with later stage procedures.
Facts about Hypoplastic Left Heart Syndrome
Infants and children who have the staged surgical procedures will require special care and treatment to support growth and nutrition. These types of heart defects also are thought to be caused by a combination of genes and other risk factors, such as things the mother comes in contact with in the environment or what the mother eats or drinks or the medicines the mother uses.
Hypoplastic left heart syndrome may be diagnosed during pregnancy or soon after the baby is born. Hypoplastic left heart syndrome may be diagnosed during pregnancy with an ultrasound, which creates pictures of the body. Some findings from the ultrasound may make the health care provider suspect a baby may have hypoplastic left heart syndrome.
This test can show problems with the structure of the heart and how the heart is working with this defect. Babies with hypoplastic left heart syndrome might not have trouble for the first few days of life while the patent ductus arteriosus and the patent foramen ovale the normal openings in the heart are open, but quickly develop signs after these openings are closed, including:. During a physical examination, a doctor can see these signs or might hear a heart murmur an abnormal whooshing sound caused by blood not flowing properly.
If a murmur is heard or other signs are present, the health care provider might request one or more tests to make a diagnosis, the most common being an echocardiogram. HLHS is a defect that also can be detected with newborn pulse oximetry screening. Low levels of oxygen in the blood can be a sign of a CCHD. Treatments for some health problems associated with hypoplastic left heart syndrome might include:.
Cardiology
Some babies and children will need medicines to help strengthen the heart muscle, lower their blood pressure, and help the body get rid of extra fluid. Some babies with hypoplastic left heart syndrome become tired while feeding and do not eat enough to gain weight. To make sure babies have a healthy weight gain, a special high-calorie formula might be prescribed.
Some babies become extremely tired while feeding and might need to be fed through a feeding tube. Soon after a baby with hypoplastic left heart syndrome is born, multiple surgeries done in a particular order are needed to increase blood flow to the body and bypass the poorly functioning left side of the heart.
The right ventricle becomes the main pumping chamber to the body. These surgeries do not cure hypoplastic left heart syndrome, but help restore heart function. Sometimes medicines are given to help treat symptoms of the defect before or after surgery. Surgery for hypoplastic left heart syndrome usually is done in three separate stages:.
Hypoplastic Left Heart Syndrome
Infants with hypoplastic left heart syndrome may have lifelong complications. They will need regular follow-up visits with a cardiologist a heart doctor to monitor their progress.
- Resources In This Article?
- Also of Interest.
- Hypoplastic left heart syndrome - Wikipedia.
- Neck and Arm Pain Syndromes: Evidence-informed Screening, Diagnosis and Management.
If the hypoplastic left heart syndrome defect is very complex, or the heart becomes weak after the surgeries, a heart transplant may be needed. Infants who receive a heart transplant will need to take medicines for the rest of their lives to prevent their body from rejecting the new heart. The images are in the public domain and thus free of any copyright restrictions.
- Egypt: Internal Challenges and Regional Stability (Chatham House Papers)?
- Hypoplastic Left Heart Syndrome HD!
- New York Politics: A Tale of Two States.
- Celebrities in Disgrace.
- Bi-directional Glenn Operation!
- Facts about Hypoplastic Left Heart Syndrome | Congenital Heart Defects | NCBDDD | CDC!